Written by Jeff Behar & copied from: mybesthealthportal.net
Being more physically active in childhood is linked to greater knee cartilage and tibial bone area in adulthood, according to new research findings presented at the 2012 American College of Rheumatology Annual Meeting in Washington, D.C.
While physical activity in childhood is often recommended as a means to improve adult joint health and function, little evidence exists to illustrate the correlation between childhood physical performance measures and bone structure in adulthood later on. The goal of the study was to determine if physical activity in youth was associated with more knee cartilage and tibial bone area (the bone that forms the distal part of the knee joint) 25 years later, says Graeme Jones, MD, PhD, investigator in the study and professor of rheumatology and epidemiology at Menzies Research Institute in Hobart, Tasmania.
Real-time data was gathered in 1985 on the childhood physical performance in a diverse group of 298 people in Australian. Of these, 48.7 percent were female and ages ranged from 31 to 41. The participant’s knee cartilage and tibial bone area were measured using T-1 weighted, fat-suppressed magnetic resonance imaging.
Although Dr. Jones and his colleagues had questionnaire responses on the physical activity level of the children taken in 1985, they found that current-day measurements revealed more accurate information.
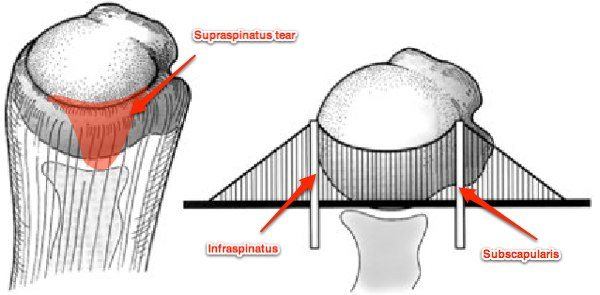
Adjustments were made for age, gender, body mass index (BMI) and past joint injuries that may affect the cartilage or bone area. The results showed that childhood physical activity, including physical work capacity, leg and hand muscle strength, sit-ups, and long and short runs had a significant, consistent association with greater tibial bone area. In addition, higher childhood physical work capacity measures were associated with greater tibial cartilage area. Other types of physical activity in childhood were associated with greater cartilage area, but these measures were less significant after adjusting for medial tibial bone area.
Dr. Jones and his colleagues do not know exactly why or how physical activity may build bone and cartilage years later. “The mechanism is uncertain, but I would contend that bone area gets larger to cope with the extra demands put on it by higher levels of physical activity, and then this lead to more cartilage, as cartilage covers the surface of bone,” he says.
While the study’s findings lend greater support to the effort in many developed countries to encourage children to be more physically active, cartilage and bone are still vulnerable to damage later on that could contribute to OA, says Dr. Jones.
“Physical activity is good, but if people have an injury while doing the physical activity, this is bad. So injury prevention is important. Avoiding a high body mass index is also important, and physical activity will help with this.”
This study was funded by NHMRC of Australia.
Get Strong! Stay Strong!
Chris